According to American Association of Neurological Surgeons, there were an estimated 157,803 cerebrovascular-related deaths in 2003; 138,397 of which were in people age 65 and older. Cerebrovascular disease is the most common life-threatening neurological event in the U.S. Intracranial atherosclerosis is responsible for approximately 40,000 of these attacks per year, representing 10 percent of all ischemic strokes. Stroke is the third leading cause of death in the United States. Of the more than 700,000 people affected every year, about 500,000 of these are first attacks and 200,000 are recurrent. About 25 percent of people who recover from their first stroke will have another stroke within five years.
Abstract
The cerebral microvessels are parenchymal branches of the brain’s penetrating vessels that include small diameter arterioles and capillaries and through which the cerebral microcirculation delivers vital metabolites to the brain. In contrast to conductance or meningeal vessels, vasomotor tone in cerebral microvessels is not dependent on the action of the sympathetic nervous system but rather on a combination of vasoreactive agents such as angiotensin, vasopressin, and purines from both brain endogenous and exogenous sources. The microvascular wall consists mainly of endothelial cells (ECs), smooth muscle cells, and pericytes (PCs) as well as the sieve-like basal lamina (BL), which together with perivascular astroglia (AS) interact dynamically to maintain the integrity and permeability of the blood-brain barrier (BBB). To ensure constant delivery of oxygen and glucose, the flow of blood through microcirculation is under autoregulatory control, both systemically and locally at the level of the microvascular wall. At the microvascular wall, endothelin (ET) and nitric oxide (NO) as well as circulating agents provide local vasopressor and vasodepressor effects that are crucial to maintain a normal vasomotor tone. Following trauma or stroke, three major pathologies occur: 1) alterations in structural integrity of microvessels and brain parenchymal cells, 2) acute edema formation, and 3) sustained hypoperfusion from vasospasm. Other pathologies that may contribute to a defective microcirculation include the formation of microthrombi and hemorrhaging, which can exacerbate the immune response. A defective microcirculation due to the loss of autoregulatory control of microvessels may contribute to the brain’s shift to anaerobic metabolism and to the formation of oxygen-free radicals, considered to be a major source of injury to nerve cells and the BBB. The diverse pathophysiologies ensuing from these events lead to nerve cell loss and poor neurological outcome. Because of these diverse pathophysiologies, monotherapeutic interventions to improve the microcirculation after trauma and stroke have had limited success both at the bench and the clinic. Recent polytherapeutic interventions aiming at improving the microcirculation as well as cell viability and neurological outcome after trauma and stroke are discussed.
Cytoarchitecture and Function of Cerebral Microvessels
The cerebral microvessels are brain parenchymal branches of the penetrating vessels and where most of the control of the local microcirculation occurs. Because microvessels lack an adventitia (outermost connective tissue layer of larger vessels), the wall of the microvessels (except for that of capillaries) consists mainly of endothelial and smooth muscle layers (Peters et al.). [1] The tube-like endothelial cells (ECs) form a continuous and single innermost layer, with apposing EC membranes closing the intercellular clefts by way of tight junctions [i.e., occluding zones, (ZOs)] that are rich in adhesion proteins such as occluding and claudin-5 (Yangand Rosenberg). [2] The muscular layer is composed of vascular smooth muscle cells (VSMCs) arranged as overlapping flat rings with long axes oriented perpendicularly to the long vascular axis (Rafols et al.). [3] In rodents, the overall cross-sectional diameter of the vessel as well as the number of concentrically arranged VSMC layers provide a morphological basis for dividing microvessels into:
- Muscular arterioles (30-100 μm in diameter; 2-3 VSMC layers),
- Terminal arterioles (10-30 μm; a single continuous VSMC layer),
- Precapillary arterioles (8-10 μm; a discontinuous VSMC layer), and
- Capillaries (5-8 μm; without VSMC but with dispersedly arranged pericytes (PCs) (Uehara et al.; Ushiwata and Ushiki; Takahashi et al.). [4],[5],[6]
Adjacent VSMCs are electrically coupled by way of gap junctions (2-3 nm in width) and constitute the main contractile element in vasoreactivity. The other contractile element in microvessels is the PC, which as VSMC expresses α-smooth muscle actin (α-SMA), desmin, endothelin (ET) receptors, and other contractile proteins. While there has been some debate over whether PC is a surrogate for VSMC in the control of vasoreactivity at the capillary level (Peppiat et al.), [7] recent morphological and immunocytochemical work has provided support for unique properties of PC in regulating blood flow through cerebral microvessels (Dore-Duffy et al.). [8],[9] In severely contracted arterioles undergoing vasospasm, scanning electron microscopy (SEM) has revealed numerous ripple-like folds or undulations on the membranes of VSMC that are roughly oriented perpendicularly to the cell long axis. Some membrane ripples in VSCM are also a feature in relaxed vessels, which may signify a state of partial vasoreactivity when maintaining normal vascular tone (Takahashi et al.). [6]
Transmission electron microscopy (TEM) studies have demonstrated the presence of a continuous, sieve-like basal lamina (BL) in the extracellular space,which intervenes between EC, PC, and VSMC as well as between VSMC and the continuous layer of astroglia (AS) endfeet (perivascular glia), which forms part of the inner glia limitans (Peters et al. Rafols et al.). [1],[3] In all capillaries, a BL is found likewise, between EC and the AS end-feet and is known to be rich in fibronectin, laminin, and matrix metalloproteinases, particularly matrix metalloproteinase 9 (MMP-9), which is thought to have a role in the degradation of the BL in brain trauma (Yu et al., Hamilton et al.). [10],[11]In addition, the BL is now thought to play a key role in the overall permeability and functional integrity of the blood-brain barrier (BBB). Originally, the function of the BBB in restricting the passage of selective molecules through most brain capillaries was thought to depend primarily on the integrity of the EC tight junctions (ZO) and an absence of EC transcellular pores. Supporting this concept is the fact that E in the capillaries of circumventricular organs, known to lack a functional BBB, exhibits transcellular pores but does not form ZOs (Benarroch). [12] Over the years, however, a functional concept of the BBB has evolved that includes not only the diffusion and transport properties of EC but also those of perivascular AS as well as the sieve-like, filtering properties of the BL intervening between EC, PC, and AS. Recently, the functional concept of a “neurovascular unit” envisions the dynamic interactions between cerebral microvessels and their functionally-associated neighboring neurons; this unit is thought to provide an integrating response not only in health but also in diseases such as TBI (Lo et al.). [13] A consequence in TBI as well as in many other neurological diseases is the compromise of the integrity of BBB and its ability to maintain a restrictive ionic milieu for the parenchyma cells of the brain, which invariably leads to the formation of edema (Chodobski et al.; Lee et al.). [14],[15]
Cerebral Blood Flow and Hemodynamics
Brain cells depend primarily on a constant supply of oxygen and glucose, their main energy metabolites, and secondarily on other metabolites, hormones, and vasoreactive substances, the passage of which is strictly regulated by the BBB. In addition, servomechanisms regulating the cerebral blood flow (CBF) provide an adequate supply of the same elements to ensure proper brain function such as maintaining nerve cell potentials. Deviation from a limited range of the standard CBF, such as that occurring after trauma or stroke, can bring about deleterious effects to the brain cells and compromise brain function. A dramatic example of this occurs after a 10-min period of brain global ischemia, which causes cessation of protein synthesis that leads to significant death of vulnerable pyramidal neurons in the CA1 sector of the hippocampus (Hossmann). [16],[17] Although longer periods of ischemia would be needed to similarly affect other brain areas, it is generally recognized that periods of less than 1 h of ischemia can irreversibly injure many nerve cells and alter synaptic circuits, leading to poor neurological outcome.
The standard unit for measuring CBF is expressed in mL of blood/100 g of tissue/min. Assuming an average brain tissue density of 1 g/mL, normal CBF in the human brain ranges approximately 50-65 mL/100 g of tissue/min, with the perfusion of gray matter (65 mL/100 g/min) being larger than that of white matter (50 mL/100 g/min) (Buxton). [18] The main force driving the CBF is the cerebral perfusion pressure (CPP), which is a pressure gradient between the mean arterial pressure (MAP) and the terminal venous plexus (TVP) and expressed as CPP = MAP-TVP (Haubrich et al.). [19] However, because of the closed nature of the cranial vault, a significant intracranial pressure (ICP) occurs, which becomes equivalent to the TVP, thus resulting in CPP=MAP-ICP, and this formula is becoming a standard for determining CPP. In order to ensure constant CBF under possible variations of CPP, brain microvessels can normally constrict or dilate to modulate CBF in response to tissue requirements, which results in a unique property of these vessels termed the autoregulation. Within a limited range, the capacity of cerebral microvessels in maintaining CBF constant, despite CPP fluctuations is called the autoregulation, which is critical for the appropriate delivery of vital metabolites to the brain (Aaslid et al.). [20]
Systemic and Local Autoregulation: Vasoconstriction/Vasodilation
Systemic and local autoregulations
Several autoregulatory mechanisms for the control of hemodynamics in the systemic circulation are well-known (Mostarda et al.). [21]Included among these are the carotid sinus and aortic arch reflexes, which detect fluctuations in blood pressure and in turn, cause the brain to modify the cardiac output and peripheral resistance, thus resulting in maintaining blood pressure within the homeostatic range (Kenny et al.). [22] Other compensatory baroreceptors located in the venae cavae, heart atria, and pulmonary vein detect systemic low pressure changes and induce increases in the secretion of brain-derived vasopressin as well as kidney-derived renin and aldosterone, which systemically result in corresponding increases in blood volume and cardiac output, ultimately normalizing arterial blood pressure (Aoyagi et al.; Mostarda et al.). [21],[23] Yet another known servomechanism is the carotid body reflex detecting changes in systemic partial pressure of carbon dioxide (pCO2) and partial pressure of oxygen (pO2), which cause compensatory changes in both respiratory and cardiac rates to maintain normal oxygenation of the brain. While these mechanisms are thought to be interdependent, the brain also provides for their integration in order to maintain homeostasis and the survival of the organism. Furthermore, while the same mechanisms form part of a systemic autoregulation that maintains CBF constant within a limited range, they are also separate from the brain’s autoregulatory control of its own local microcirculation. Thus, the ability of the brain to autoregulate CBF through its microcirculation is to a great extent, albeit not solely, dependent both on physicochemical properties of the microcirculation and the specialized functions of VSMC and EC that reside in the microvascular wall (Rafols et al.). [3] Thus, in contrast to VSMCs in the muscle layer (tunica media) of large or extraparenchymal conducting vessels, VSMCs in brain microvessels (or resistance vessels) lack sympathetic innervation and are thus, not influenced by generalized sympathetic-driven responses, as are those occurring in meningeal vessels or those forming part of the systemic circulation. Without this “neurogenic” control, hormones and purines as well as fluctuations in CPP can normally alter the reactivity of brain microvessels, thus affecting the flow of blood through the microcirculation. For example, within a limited range of fluctuating CPPs, the cross-sectional diameter of a cerebral microvessel can increase or decrease, as needed in order to maintain appropriate CBF for the delivery of needed metabolites to the brain parenchyma. Likewise within this limited range, a sudden increase in CPP may result in a compensatory decrease in the cross-sectional area of the microvessel, which then would lead to increased vascular resistance, thus preventing hyperemia and excess oxygenation of the parenchyma. Conversely, a state of hypoxia and hypercapnia may induce an increase of the microvessel diameter, which in this case would lead to greater oxygenation of the brain. These autoregulatory responses are part of the brain’s capability to maintain constant delivery glucose and oxygen for normal function. In the systemic circulation, similar VSMC effects can be obtained from agents such as vasopressin, angiotensin, ET, adenosine, cyclic adenosine monophosphate (cAMP), and nitric oxide (NO), to name a few. A generalized review of vasoreactivity and how the above factors can affect vasoconstriction and vasodilation follow.
Vasoconstriction
In peripheral vessels, the degree of contraction of VSMCs in the muscle layer determines the extent of vasoconstriction, this action causing a decrease in the lumen of the vessel concomitant with a decrease in blood flow, which brings about an increase in peripheral resistance of the vascular bed and a rise in blood pressure (Mandell et al.). [24] In peripheral vascular beds, the release of nor-epinephrine (NE) from sympathetic nerve terminals as well as circulating epinephrine (E) initiate vasoconstriction, with NE and E binding to a family of adrenergic receptors in the membrane of VSMC. While not all VSMCs receive direct innervation by autonomic nerves, the electrotonic coupling (i.e., gap junctions) among VSMCs causes a spreading depolarization to the neighboring cells. A signal transduction cascade in VSMC then causes intracellular calcium and inositol triphosphate (IP3) to be released from the sarcoplasmic reticulum. Phosphorylation of the light-chain myosin kinase (LCMK) by activated calmodulin causes cross-bridge cycling between the contractile proteins, which results in the shortening of circularly arranged VSMCs (Lapointe and Buret), [25] thus decreasing the overall vessel diameter. Though during contraction VSMC in brain parenchyma microvessels use a similar signal transduction mechanism, because of their lack of direct autonomic innervation, the initiation for this contraction depends on physical and molecular events taking place locally across the vascular wall. Specifically, rheostatic (e.g., perfusion pressure, blood viscosity) and humoral (circulating vasoactive agents) events at the luminal membrane of EC may initiate a signal transduction cascade of molecular events, which are transmitted across EC and ultimately influence the contractility of VSMC. While many circulating vasoactive agents may initiate vasoconstrictive effects in cerebral microvesels, the actions exerted by vasopressin, angiotensin-II, and ET-1 are particularly notable. Vasopressin is produced in the hypothalamus and stored in the posterior pituitary wherefore once released, it causes water retention through the distal and collecting tubules of the kidney. Vasopressin systemic vasopressor effects both in peripheral blood vessels and in cerebral vessels have been recognized. In the brain vasopressin has been implicated in memory formation, retention of both short and long-term memories (Bosch and Newman, Stevenson and Caldwell), [26],[27] temperature regulation, and blood pressure regulation (Lim and Young). [28] Another systemic vasopressor, angiotensin (Ang)-II with its receptor AT1, have been localized to hypothalamic nuclei such as the supraoptic and paraventricular nuclei, lamina terminalis, lateral parabrachial nucleus, ventrolateral medulla, and the nucleus of the solitary tract (NTS) where they may play a role in the central control of water balance and blood pressure (Aoyagi et al.). [23] Furthermore, Ang AT1 receptor antagonism strongly affected the brain circulation and normalized profound alterations in cerebrovascular structure and function, characteristic of chronic genetic hypertension (Saavedra). [29] In addition, the Ang AT 2 receptor has been localized to ECs in cerebral microvessels where it may act to control CBF from circulating Ang originating from both brain endogenous and exogenous sources (McKinley et al.). [30] Generally for most vascular beds, the most powerful vasoconstrictor found to date is ET-1, thought to have 10 times the vasoconstrictive action of Ang-II. As in most vascular beds, brain ET-1 is a small (21AA) peptide primarily synthesized in EC (Yanagisawa et al.) [31] where by binding to its two major receptors, ETrA and ETrB, it may play a significant role in the control of the local microcirculation. While brain ETrA has been localized primarily to VSMCs and neurons, ETrB appears to have a wider distribution that includes EC, VSMC, and neurons (Kallakuri et al.). [32] The role of ET-1 in neurons and other brain cells remain to be elucidated, though a signaling role of ET-1 in the neurovascular unit has been postulated. As will be elaborated later, while selective ETrA blockade in the brain was shown to mitigate traumatic brain injury (TBI)-induced hypoperfusion, a similar selective blockade of ETrB had little effect in the TBI-induced hypoperfusion (Kreipke et al.). [33]
Vasodilation
Relaxation of VSMCs in the tunica media brings about an increase in the cross-sectional diameter of the vascular lumen (i.e., vasodilation), concomitant with an increase in blood flow and decreases in vascular resistance and blood pressure. Because of the inherent contractility of VSCM to maintain a normal vascular tone and blood pressure, true vasodilation may occur when VSMC relaxes way above the level required to maintain baseline vascular tone. In this case, vasodilation can bring about corresponding changes in peripheral resistance, cardiac output, and arterial pressure. Neurogenic vasodilation of peripheral vessels is mostly controlled within the central nervous system via the central inhibition of vasopressor (and cardio-accelerator) centers located in the medulla of the brainstem. Thus, a decrease in sympathetic impulses below the level required to maintain baseline vascular tone may lead to VSMC relaxation and increases in the cross-sectional diameter of the vessel (i.e. vasodilation), which would facilitate blood flow and decrease peripheral resistance. In addition to this, neurogenically-mediated vasodilation and blood-borne vasodilating agents in the circulation are known to directly control the relaxation of VSMC. These have been classified into three classes using distinct mechanisms of action: 1) c-AMP-mediated eicosanoids such as prostaglandin (PG)12; 2) hyperpolarizing-inducing types such as adenosine through calcium channel blockers; and 3) cyclic guanosine monophosphate (GMP)-mediated nitrovasodilators such as NO (Fusco et al.). [34] All three types are thought to have roles in the control of the cerebral autoregulation.PG12 is secreted by EC in a paracrine fashion and upon binding G-protein receptors (Morgado et al.), [35] it activates adenylyl cyclase and production of cytosolic cAMP. An increase in cAMP levels then causes activation of protein kinase (PKA) and inhibition of the myosin light-chain kinase (MLCK), which allows relaxation of VSMC (Velero et al.). [36] In contrast, adenosine exerts vasodilatory effects by acting through voltage-gated calcium channels (Petrov et al.). [37] Adenosine increases also the diameter of coronary vessels, thus improving blood circulation to the heart. In brain adenosine is thought to be an inhibitory transmitter which normally suppresses arousal and promotes sleep. Finally the most widely studied cyclic(c) GMP-mediated vasodilator is NO, a gas which plays a significant role in the vasodilation in peripheral vascular beds. Originally, NO was known as the endothelium-derived relaxing factor (EDRF) and in the brain, it can be synthesized by a family of three NO synthases, endothelial NOS (eNOS), neuronal NOS (nNOS), and inducible NOS (iNOS). In peripheral beds, NO when released quickly diffuses across EC membranes and the extracellular space to reach VSMC, causing it to relax (Mayo et al.). [38] Its mechanism of action is initiated by NO stimulation of guanylate cyclase production of cGMP in VSMC. Increased cyclic guanidine monophosphate (cGMP) then activates protein kinase G, which causes calcium reuptake into the sarcoplasmic reticulum and opening of calcium-activated potassium channels. The fall in calcium concentration ensures that MLCK can no longer phosphorylate the myosin molecule, thus inhibiting cross-bridge cycling between contractile filaments, which leads to VSCM relaxation (Chung et al.; Islam et al.). [39],[40] Finally attenuation of iNOS messenger RNA (mRNA) (inducible NO synthase is a critical enzyme for NO synthesis) exacerbates the TBI-induced hypoperfusion and upregulates ET-1 expression in the hippocampus and cortex (Steiner et al.), [41] suggesting that NO may interact with ET-1 in the dysfunctional microcirculation after trauma (see also below).
Types of Traumatic Brain Injury Pathologies and Related Pathophysiologies
Types of traumatic brain injury
TBI remains a major cause of disability among individuals under 40 years of age, contributing to 30.5% of all injury-related deaths in the USA alone (Langlois et al.). [42] Of the 1.7 million people sustaining TBI in the USA alone, 275,000 required hospitalization with 52,000 resulting in death (Faul et al.). [43] Because of the heterogeneous nature of causes leading to head injuries, TBIs have been generally classified into two broad categories. The first encompasses open-head brain injuries that are accompanied by skull fractures and disruption of the meninges. In this case, physical damage directly to the brain from a contusion (bruising) or laceration (tearing) together with varying degrees of hemorrhaging outside and inside the brain may occur. A second major category includes closed-head brain injuries without penetration of the skull or meninges. In this second category, bleeding is less severe and may be restricted to the meningeal layers and the perivascular spaces of the parenchyma. TBIs from this latter category are the most common, as they have a wide range of causes, from head bumps, concussions, shaking, to acceleration/impact injuries such as those resulting from falls in the elderly population or those incurred during sports or car accidents. The diversity of TBI causes and their ensuing heterogeneous injuries led to the development of the Glasgow Coma Scale in 1974 (Teasdale and Jennet), [44] which allowed accurate reading of the conscious state of the patient. More recently, the Neurological Outcome Scale for Traumatic Brain Injury (NOS-TBI) is thought to provide a more accurate assessment for the treatment and rehabilitation of TBI patients (Wilde et al.; McCauley et al.). [45],[46],[47] Because of the extensive TBI research literature accumulated in the last two decades, this review first summarizes information on the most common types of injury and then focuses on events related to the second category of injuries (i.e., closed-head injuries).
Because of the TBI diversity mentioned above, finding a suitable TBI experimental animal model to replicate some of the neurological issues encountered in the clinics has been problematic. Generally, three TBI models have been widely used and considered as validated:
- Lateral fluid percussion,
- Controlled cortical impact, and
- Impact acceleration model. In the lateral percussion model, after trepanation of the skull, a pressurized pulse of saline solution is delivered against the surface of the dura mater (McIntosh et al. Morales et al.). [48],[49]
While data from this model are applicable only to certain open-skull (i.e., penetrating) injuries, it would not be useful to study effects from the more commonly occurring closed head injuries seen in the clinics. In the controlled cortical impact model (Dixon et al.), [50] a force-controlled piston impacts directly the surface of the brain, which also makes the model an open-head injury type. Apart from having the limitations of the first model, injury sites with this model usually exhibit substantial tissue necrosis and extravasation of blood (i.e. hemorrhages), which are much less severe in closed-head models. Finally, the impact acceleration model (Foda and Marmarou, Marmarou et al.) [51],[52] derived from an earlier weight drop model, uses a known weight dropped onto the surface of the skull from selected heights. The utilization of a steel “helmet” and underbody foam pad ensures integrity of the skull and consistency in the delivery of impact, thus mirroring the acceleration-deceleration phenomena associated with closed-head injuries as seen in many TBI patients (Foda and Marmarou, Rafols et al.). [3],[51] In addition, this model reliably yields both robust diffuse axonal injury (DAI) and alterations in the brain microcirculation, both of these pathologies commonly seen in patients who have sustained closed-head injuries (Rafols et al.). [3]
Pathologies and Related Pathophysiologies in Traumatic Brain Injury
Regardless of whether a TBI is of the closed-head or open-skull variety, all TBIs lead to three major pathologies:
- Structural damage to neurons, neuronprocesses (e.g., dendrites, axon), glial cells, and cellular components of blood vessels,
- Inflammation and metabolic alteration such as edema, and
- Sustained vasospasm and loss of the local autoregulation of the microcirculation.
The sustained vasospasm and diminished flow of blood through the microcirculation brings about a state of hypoperfusion of the brain parenchyma that can last from hours to days after the traumatic event (Bouma and Muizelaar, Morales et al., Coles et al., Inoue et al., Oertel et al.). [49],[53],[54],[55],[56] Under prolonged hypoxia, brain cells and synaptic circuits are compromised, which may impact on lasting behavioral deficits and neurological outcome. Other pathologies such as petechial (e.g., perivascular) bleeding and formation of microthrombi or capillary plugs have been observed in several trauma models. An important distinction related to the development of the injury would be whether these pathologies develop immediately after initial trauma or over time, which results in the recognition of the “primary injuries” and “secondary injuries.” Thus, a “primary injury” is the result of mechanical force applied to the brain tissue, which acutely produces direct injury to neurons, neuronal processes, glia cells, and blood vessels. However, while such injury usually brings about the pathologies mentioned above, some of their associated pathophysiologies and deleterious effects may not develop immediately but over the course of time, which may lead to accruement of primary tissue damage, thus resulting in the “secondary injury.” As the time window between primary and secondary injuries can be in the order of weeks to months (and sometimes years), much research today is designed to develop therapeutic interventions to prevent the development of secondary injuries. An example of primary and secondary injuries may relate to events associated with a focal contusion to the brain. Thus, at the side of impact, the primary injury would primarily consist of an area that would include rapidly dying nerve cells, glia cells, and vascular cells, together with varying degrees of hemorrhaging, the extent of this injury being proportional to the severity of the impact. However, in the course of time, a secondary injury affecting areas close or distant to the primary one would ensue, in this case its extent determined by the severity of the primary injury.
Documented morphologic alterations to neurons, their processes, and to blood vessels include changes in the normal ultrastructure of the nerve cell body, dendrites, and the axon (Marmarou et al.; Rafols et al.; Kallakuri et al.). [3],[32],[52] Morphological alteration of the cytoskeleton in the dendrites and axon with accompanying loss of shape and orientation of the processes has been widely observed. The most prominent in concussive, closed-head type injuries is the occurrence of diffuse axonal injury (DAI). As early as 1956, diffuse degeneration in white matter bundles that lead to permanent incapacitation was found in human patients with closed-head injuries (Strich). [57] Subsequent TBI studies demonstrated a correlation of injury severity with white matter integrity (Arfanakis et al.; Gupta et al.; Inglese et al.; Benson et al.; Rafols et al.; Wang et al.; Marquez de la Plata et al.). [58],[59],[60],[61],[62],[63],[64] The pathophysiology leading to DAI has been reviewed by Povlishock (2006). Briefly shearing forces transmitted through the brain after impact is thought to cause permeability changes and increased membrane poration of axons in the long tracts of white matter. Signal transduction then would lead to elevated intracellular calcium, activation of cysteine proteases such as calpain, degradation of neurofilaments, and ultimate fragmentation of the axon (Povlishock and Karz; Buki and Povlishock). [65],[66] Another cause for DAI may be a secondary effect from the state of hypoperfusion immediately after TBI (see below). Thus, under insufficient oxygen delivery and increased anaerobic glycolysis, lactic acidosis accumulates, which alters membrane permeability due to the formation of reactive oxygen species (ROS) species and lipid peroxidation of membrane unsaturated fatty acids. As a consequence of these cellular and molecular events, the ensuing anterograde (i.e., Wallerian) axonal degeneration would lead to destruction of axon terminal branches, synaptic loss, and disruption of neural circuits underlying cognitive, sensory, and motor impairments afflicting many TBI patients.
A second major pathology after TBI is the formation of edema, an acute event, which has been classified into cytotoxic and vasogenic types (Marmarou et al.). [67] Thus, vasogenic edema after TBI may occur from either mechanical (e.g., disruption of tight junctions) or metabolic alterations [e.g., failure of adenosine triphosphate (ATP)-dependent osmotic pumps] of the BBB, which allows for the osmotic gradient transfer of fluids and solutes across the microvascular wall, that is, between blood plasma and the extracellular compartment around blood vessels (DeWitt and Prough; Unterberg et al.). [68],[69] In contrast, cytotoxic edema affecting primarily the volume of cells is the accumulation of fluid passing from the extracellular to intracellular compartments of nerve cells and AS due to a failure in membrane permeability (Stifel et al.; Chen and Swanson; Unterberg et al.). [69],[70],[71] Brain swelling from edema and failure of reabsortion of fluids into the circulation are the main reasons for the sharply elevated ICP found after trauma. Cytotoxic edema and increased ICP develop within minutes following TBI and if unresolved, can lead to herniation, pressure coning on brainstem respiratory and cardiovascular centers, and cessation of breathing and cardiovascular function, which become critical morbidity issues in the acute care of TBI patients. Paradoxically provided that severe edema is resolved, it usually does not lead to significant cognitive impairment.
The third major pathology after TBI has been the least investigated to date and relates to alterations in CBF and the microcirculation that are initiated within minutes following onset of the traumatic event. Thus, within the last 30 years, experimental and clinical data demonstrated fluctuations in CBF and altered autoregulation of the microcirculation after TBI. Specifically in closed-head injuries as well as after direct impact of the brain, a state of sustained hypoperfusion independent of brain swelling has been observed to last from hours to days following impact (Abu-Judeh et al., Petrov and Rafols, Steiner et al., McBeth et al., Rafols et al.). [3],[41],[72],[73],[74] Although this theme is further elaborated in the next section, it is sufficient it to say that prolonged, insufficient perfusion and reduction of vital metabolites to the brain are thought to impact not only on the structural integrity of neurons, glial cells, and microvessels but also on the integrity of the BBB already damaged in the primary injury. Other morphological changes of cerebral microvessels in the form of constricted capillaries and PCs as well as diffuse formation of microthrombi have been documented in several models of TBI (Hekmatpanah and Hekmatpanah, Foda and Marmarou, Dore-Duffy et al., Rafols et al.) [3],[51],[75],[76] and may exacerbate the local hypoperfusion discussed above. Taken together, it is reasonable to envision the interrelatedness of these pathologies and how their associated pathophysiologies might contribute to the development of the secondary injury where the hope for therapeutic intervention lies.
Microcirculation and the Endothelin System in Traumatic Brain Injury
Experimental models of brain trauma have revealed morphological alterations of brain microvessels as well as decreases in CBF that are temporally associated with neuronal injury and reduced cognition (Armstead; Rafols et al.; Kreipke et al., Kreipke et al.). [3],[31],[77],[78]Specifically using the impact acceleration model, TEM analysis revealed EC shape distortion and collapse of the microvascular lumen, thickening of the BL intervening between EC and VSMC, evidence of VSMC enhanced contractility, and swelling of AS end-feet that coincided temporally with a 37% decrease in the CBF, as measured by laser Doppler flowmetry (Rafols et al.). [3] While some of these alterations have been interpreted as being caused by shearing forces generated by the trauma (Foda and Marmarou; Rodriguez-Baeza et al.), [51],[79] visual evidence of VSMC contraction strongly suggests alteration of normal vascular tone and loss of autoregulatory control, thus explaining the posttraumatic state of hypoperfusion. Similar CBF-induced alterations were previously documented in other rat models of TBI (Yuan et al.; Yamakami and McIntosh; Muir et al.), [80],[81],[82] as well as in humans (Martin et al.). [83] Additionally, in rodents, the critical threshold of hypoperfusion needed to develop irreversible tissue damage is approximately 15-20 mL/100 g/min (Bramlett and Dietrich). [84] Following severe head trauma in humans, vasospasm of the large conductance brain vessels occurs concomitant with dilation of the resistance vessels (Martin et al.; Lee et al.). [83],[85] In their prospective transcranial Doppler study in humans after severe closed injury, Martin et al. [83] found that the dilation of resistance vessels occurred at least between 4 days and 15 days after trauma, which is at a time much later than the hypoperfusion phase seen both experimentally and clinically lasting 48 h after trauma (Petrov and Rafols, Steiner et al.). [41],[86] This hypoperfusion has been related to the impaired hypertensive cerebral autoregulation after brain trauma (Lewelt et al., Dewitt et al., Armstead and Kurth, Endelborghs et al.). [87],[88],[89],[90] However, the precise mechanism that may underlie this defective autoregulatory control is yet to be fully elucidated. Previous work from our laboratory and that from others have implicated the role of ET-1 in the autoregulatory control of these vessels (Zhang et al. 2000, Petrov and Rafols, Steiner et al., Petrov). [41],[86],[91] ET-1 is a powerful vasoconstrictor found in EC, glia, invading macrophages and neurons (Yanagisawa et al.; Zimmerman and Seifert; Masaki) [31],[92],[93] and in peripheral VSMC. ET-1 mediates vasoconstriction through its ligand-gated ETrA and ETrB receptors (Andersson; Granchi et al. 2002). [94]After TBI, ET-1, ETrA, and ETrB levels increase (Steiner et al., Armstead and Kreipke). [41],[95] Furthermore, spatial alterations in the expression of these receptors have been temporally associated with the altered microcirculation after TBI (Kallakuri et al.). [32] Thus, ETrA was more prominently expressed in cortical pyramidal neurons at 2 h and 48 h after trauma while it reached its peak in microvessels at 4 h, which corresponds to the times of significant ET-1-mediated vasoconstriction (Steiner et al. 2004, Armstead and Kreipke, Kreipke et al.). [41],[95],[96] In contrast, ETrB was expressed prominently in EC, VSMC, PC, and perivascular neurons at 24 h after trauma, which may signal also a role for this receptor in vasoreactivity (Kallakuri et al.). [32] However, the precise molecular signaling involving ET-1 and how it may induce VSMC contraction remain unclear. Some evidence suggests that calponin, an actin-binding protein may participate in ET-1-mediated VSMC contraction (Gimona and Small, Winder and Walsh, Yang et al. 2004, Kreipke et al. 2007); [78],[97],[98] however, more work using TBI models is needed in this area.
Therapeutic Modulation of the Endothelin System After Traumatic Brain Injury
Armstead [77] first demonstrated that TBI-induced vasoconstriction of pial microvessels could be abated following ETrA antagonism with BQ-123, a selective ETrA antagonist. ET-1 was also shown to blunt KATP channels, thereby reducing NO- and cGMP-mediated vasodilation. In contrast, BQ-123 antagonism ameliorated channel dysfunction, suggesting that at least in pial arterioles, ET-1 alterations after TBI may be involved in decreased vasodilation in addition to vasoconstriction (Kasemsri and Armstead). [99] More recently the role of ET-1 and its modulation in neurological disorders has gained support (Armstead, Grasso, Armstead and Kreipke 2011), [95],[100],[101] as the occurrence of cerebral vasospasm in patients with brain injury has been correlated with increased levels of ET-1 in CSF and plasma (Lampl et al., Beuth et al., Mascia et al., Salonia et al.). [102],[103],[104],[105] However, the modulation of ET-1 and its receptors to ameliorate the pathologies encountered after TBI needs to be more thoroughly investigated. Using BQ-123 and BQ-788 (a selective ETrB blocker), Kreipke et al. [33]showed differential effects of ETrA and ETrB on TBI-induced cortical cell injury and hypoperfusion. In that study, BQ-123 or BQ-788 were administered intracerebroventricularly and CBF was assessed in the sensorimotor cortex with arterial spin labeling magnetic resonance imaging (ASL-MRI), whereas the degree of cortical cell injury was determined by fluoro-jade (FJ) labeling and morphometry. As such, BQ-123 caused amelioration of the TBI-induced hypoperfusion and reduced the number of FJ-labeled cells at 24 h and 48 h after trauma while BQ-788 had no significant effect on either hypoperfusion or FJ-labeling (Kreipke et al.). [33],[96] Differential effects in behavioral outcome after TBI were also obtained by selective modulation of the same receptors using BQ-123 and BQ-788 (Reynolds et al.). [106] In addition to its beneficial vasoreactive effects, ET-1 modulation may ameliorate another TBI-induced pathology. Thus, BQ-123 reduced the extent of diffuse axonal injury in corpus callosum at 24 h and 48 h after TBI (Reynolds et al.). [107] However, it is unclear to date whether the above BQ123 effects on DAI and cell injury might occur directly on the injured nerve cells and their axons or indirectly by an initial resolution of the TBI-induced vasospasm and hypoperfusion, which then might cause the decrease in DAI. To date, no clinical trial has been aimed at addressing the endothelin system after TBI and more basic research on ET-1 and its receptors must be performed at the bench level before therapeutic intervention by modulation of this system can be brought up to clinical trials.
Stroke: Ischemic Core and Penumbra
Stroke
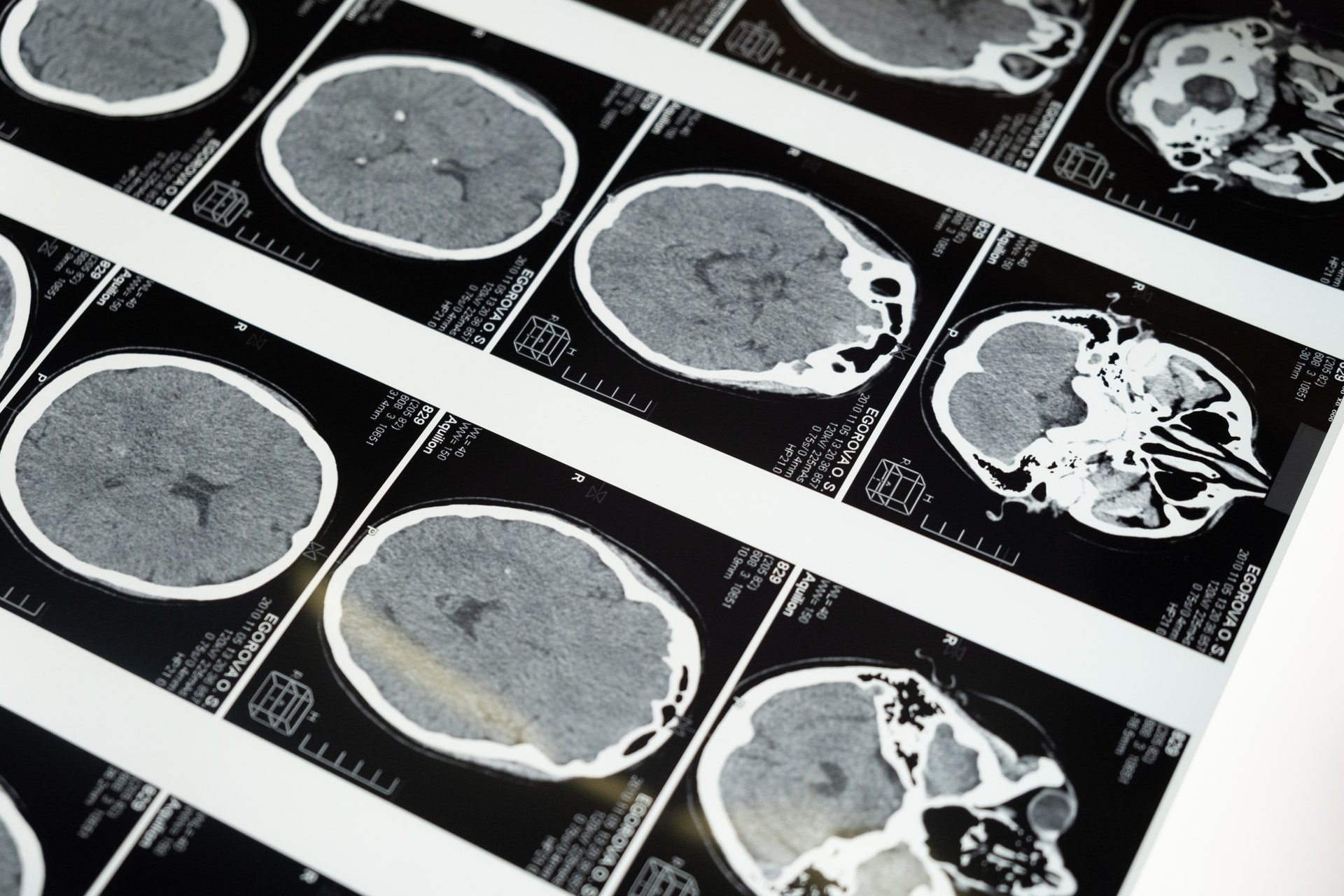
In 2010, approximately 17 million people worldwide were victims of stroke (also known as cerebrovascular accident or CVA), which is ranked after heart disease and before cancer as a major cause of death and disability (Donnan et al.). [108] Strokes are broadly classified into two major categories: Ischemic and hemorrhagic, with 87% of strokes being ischemic and the rest hemorrhagic (Feigin et al.). [109] Because of the present review’s scope and based on similarities between ischemic stroke events with those occurring in closed-head brain injuries, the following discussion will focus mainly on ischemic stroke and reviews dealing with similar events in other strokes should be consulted elsewhere.
Etiologies in ischemic stroke can be complex and derived from diverse pathologies originating from both within and outside of the brain. However, invariably, events leading to an ischemic stroke may stem from the development of a clot (or thrombus) locally, elsewhere in the body (embolism), systemic hypoperfusion (shock), or venous thrombosis. The majority of ischemic strokes are further caused when a thrombus causes a partial or total obstruction in the lumen of a major cerebral arterial vessel [e.g., the middle cerebral artery (MCA)], which results in a decreased blood flow to the territory of the brain supplied by the obstructed artery (in the case of the MCA, nearly the entire lateral aspect of the ipsilateral cerebral hemisphere). Deprived of oxygen and other vital metabolites, an ischemic cascade (Fisher and Ginsberg, Deb et al.) [110],[111] will be initiated with catastrophic consequences to the oxygen-deprived area, leading to metabolic dysfunction, cell death, and tissue infarction, the severity of which is directly related to the intensity and duration of the ischemic insult (del Zoppo and Garcia). [112] Moreover, experimental and clinical experience attest to the fact that the severity of the stroke in terms of its volume and irreversible tissue infarction directly correlate with the degree of impairment in cognitive, sensory, and motor functions, which usually afflict stroke patients.
Ischemic Core/Penumbra
Despite the possibility of extensive cell death and tissue infarction following a stroke, experimental focal ischemia models have revealed heterogeneous cell death and tissue preservation throughout the ischemic zone, which has brought about the concept of the ischemic “core” and “penumbra” (Fisher and Ginsberg). [110] Thus, at its center or “core,” due to severe hypoxia or even anoxia, the CBF may drop to below 8-10 mL/100 g/min, which leads to necrotic cell death of neurons as well as that of neighboring glia and vascular cells within minutes to a few (4-6) hours following the stroke’s onset. In contrast, around the core or ischemic boundary zone, a circumferential area of tissue known as the “penumbra” undergoes less severe hypoperfusion with a reduced CBF approximately ranging 13-20 mL/100 g/min from collateral blood vessels (Hakim). [113] To some extent, this sustained hypoperfusion mirrors that occurring in impact-acceleration, closed-head models of TBI, as described in Section IV of this review. Under hypoxic stress, many penumbral cells would be vulnerable to death if no intervention (e.g., recanalization by thrombolysis or thrombectomy) is performed within the available narrow window (usually 6-8 h). In addition, because many cells in the penumbra may not be irreversible injured, it is in this area where the main focus of intense investigation is centered for transitioning from injury to repair after stroke (Eng). [114]
The Microcirculation After Stroke
Analyses of penumbra cells and blood vessels reveal pathological events not unlike those described for TBI in Section IV. Thus, evidence for structural alterations of nerve cells, supporting cells and/or microvessels, metabolic changes with edema formation as well as a state of sustained hypoperfusion through the microcirculation, coupled with constriction of VSMC, EC, and PC have been substantiated in histological studies of the penumbra (Garcia and Kamijyo, Dirnagl et al., Muller et al., Haberl, Zhang et al.; Morris et al.; Ding et al.; Yemisci et al.). [115],[116],[117],[118],[119],[120],[121],[122],[123] In embolic stroke, these ischemic changes can be exacerbated if recanalization of the obstructed vessel and restoration of the blood flow are affected, which may then lead to reperfusion injury (Ginsberg, Clark et al., Aronowski et al.). [124],[125],[126] However, despite strong evidence confirming the above alterations of the microcirculation and CBF in focal models of ischemia, there has been little evidence ascertaining real-time observation of vasoreactive changes in stroke. Thus, in a rat model of global ischemia and reperfusion, Takahashi et al. [6] used correlative laser Doppler flowmetry and SEM to demonstrate enhanced VSMC contractility of brain parenchymal arterioles and precapillary arterioles, which temporally coincided with the phase of hypoperfusion. In addition, increased arteriolar contractility and significant blood flow reduction with decreased vascular density in the microcirculation were directly observed in patients during aneurysm surgery or decompressive craniectomy after stroke (Pennings et al., Perez-Barcena et al.). [127],[128] It is now thought that the above morphological alterations impact not only the regional microcirculation of the ischemic tissue but ultimately the extent of cell injury in the penumbra. To that extent, Dalkara et al. (2012) showed intermittently spaced (or nodal) capillary constrictions which colocalized with luminal microthrombi (or capillary plugs) as well as with α-SMA labeled PCs, suggesting a heterogeneous involvement of penumbral tissue via a defective microcirculation. This heterogeneous capillary nodal constriction throughout the ischemic tissue may further explain the “no reflow” phenomenon, even after complete recanalization following thrombolysis (Dalkara et al. 2012).
Another prominent pathology in the microcirculation in postcapillary venules is the accumulation of leukocytes in the cerebral microcirculation during early reperfusion (del Zoppo et al., del Zoppo and Garcia, Ritter et al., Ding et al.). [112],[122],[129],[130] Generally, it is thought that ischemia triggers the expression of cytokines, which attract leukocytes into ischemic sites with subsequent induction of intercellular adhesion molecule (ICAM)-mediated leukocyte adhesion to the luminal wall of microvessels. Following adhesion, many leukocytes migrate through the vessel wall (leukocyte rolling) into the brain parenchyma (Okada et al., Wang et al., Garcia et al. 1994). [131],[132] This phenomenon is considered to be a major trigger for the acute inflammatory response that follows after stroke. Experimentally, Ding et al. [122] used saline infusion into the ischemic territory prior to reperfusion as a way to decrease vascular plugging, this procedure ameliorating both the inflammatory response and infarct volume. Other strategies involving antileukocyte adhesion therapies have been used with varying degrees of success (Clark and Zivin, DeGraba) [133],[134] and will be further elaborated in the next section.
Finally, oxidative damage in ischemia and reperfusion has received significant attention in stroke research. Early brain ischemia studies supported a role for ROS in the development of cell and vascular injury, particularly during early reperfusion (Jenkins et al., Watson et al., Bromont et al., Sakamoto et al., Welsh et al.,Traystman et al., White et al.). [135],[136],[137],[138],[139],[140],[141] More recent work has extended this concept by attributing excessive ROS formation to a metabolic dysfunction precipitated by reduced oxygen and glucose in ischemia followed by a burst of oxygen during early reperfusion (Abramov et al., Ozkul et al., Suh et al., Pradeep et al., Tang et al.). [142],[143],[144],[145],[146] Thus, under conditions of severe hypoxia or anoxia, energy sources (ATP) in brain cells are rapidly depleted, resulting in failure of ion pumps critical to maintain ion gradients, which lead to impairment of not only nerve cell potentials but also increased permeability across the BBB. Furthermore, because a persistent state of anaerobic glycolysis, nerve cells enter into a state of lactic acidosis and overproduction of arachidonic acid, which leads to increased ROS formation. Elevated ROS has also been associated with lipid peroxidation of membrane unsaturated fatty acids, proteolysis, and even DNA impairment. Even if recanalization after ischemia is successful, these abnormalities can be further compounded by the sudden burst of oxygen recirculating through the anoxic tissue during early reperfusion, which results in exacerbation of ROS formation. Thus, excessive ROS formation during ischemia/reperfusion is now considered a critical issue in cell injury and BBB dysfunction after stroke and inhibiting ROS production and its deleterious effects after stroke has become a primary target of many current and future therapies.
Pathophysiology and Therapeutics
Because of the multiple pathologies occurring in embolic stroke, it is not difficult to realize why most monotherapies used in the past have had such little effect on improving the neurological outcome. While hypothermia and induced barbiturate coma have had limited success in inhibiting some of the deleterious effects of the ischemia-induced metabolic dysfunction, which would include lactic acidosis and ROS formation, these therapies can be cumbersome to implement and do not provide lasting benefits (Barone et al. 1997, Colbourne et al., Cornet et al. 2012, David et al. 2012). [147] The Food and Drug Administration (FDA)-approved recombinant tissue plasminogen activator (r-tPA) has also had some success in a small percentage of embolic stroke patients, as it has a narrow window and little effect if administered after 6 h from stroke onset. Normobaric oxygen is also considered as an effective way to reoxygenate the anoxic brain and can be easily administered to stroke patients. However, at levels above 60%, it is thought to increase the accumulation of ROS in cells, which could potentially exacerbate tissue damage, thus worsening outcome. Experimental studies strongly suggest that improving the microcirculatory flow after recanalization (or even if recanalization fails after rt-PA therapy) may be the most effective way for improving outcome (Dalkara et al. 2012). The assumption here is that if flow through the microcirculation can be reestablished within hours prior to reperfusion, it could reoxygenate ischemic tissue and salvage many penumbral cells that would otherwise be destined to death. To achieve this goal, it would be paramount to blunt the formation of capillary plugging and leukocyte adhesion/rolling across endothelial membranes by using leukocyte antiadhesion molecule strategies. To that extent, several experimental therapeutic approaches have been carried out with moderate success. Saline infusion into an ischemic territory before reperfusion was found to reduce capillary plugging and inflammatory injury, and improve neurological outcome (Ding et al.). [122] In addition, reduction of capillary plugging by pharmacological or genetic manipulation that inhibited leukocyte adherence, platelet activation, or clot formation has been shown to restore the microcirculation after stroke (Mori et al. 1992, Schulz et al. 1997, Ishikawa et al. 2005, Yemisci et al.). [123] In parallel work to improve oxygenation of the vascular bed after stroke has focused on angiogenesis or the development of new capillary branches from the existing ones (reviewed by Ergul et al.). [148]Angiogenesis after stroke has been found to be a transient phenomenon in the penumbra, which has been associated with neurogenesis and which can be augmented by both pharmacological intervention such as erythropoietin (EPO) and nonpharmacological intervention such as exercise. Thus, EPO enhanced neurogenesis and angiogenesis at the stroke boundary by increasing levels of brain-derived neurotrophic factor (BDNF) and vascular endothelial growth factor (VEGF) (Wang et al., Reitmeir et al.) [149],[150] and similar angiogenic effects and increased synaptic plasticity have been obtained by the implementation of exercise regimes prior to or after stroke (Gertz et al., Davis et al., Zhang et al.). [151],[152],[153] However, dose-limiting toxicity and drug delivery barriers have tempered the development of EPO as a stroke therapy (Rem and Finklestein, Ehrenreich et al.). [154],[155] Antioxidant strategy to modulate signal transduction events leading to ROS formation before or after stroke appears to be also very effective in reducing ROS accumulation within vascular and inflammatory cells and in improving neurobehavior outcome (Tang et al., Weston et al., 2012). [156],[157] Progesterone in experimental permanent stroke as well as after trauma likewise appears to be neuroprotective (Stein) [158] and promote BBB integrity by inhibiting the inflammatory cascade and reducing both BBB metalloproteinases and degradation of tight junction proteins (Stein, Wali et al.). [158],[159] However, to date, the therapeutic value of progesterone in stroke or trauma clinical trials has yet to be validated. A more promising therapy particularly in the chronic period after stroke, appears to be the use of stem cell (or cell-based) strategy. Thus, bone marrow mesenchymal stromal cells exerted therapeutic effects by reducing infarct volume if delivered 3 days after stroke (Komatsu et al., Yang et al.), [2],[160] and based on these findings, investigators have recommended careful translation of this strategy to patients regarding protocols, dosages, cell characterization, underlying mechanisms of actions, and outcome measures (Savitz et al., Savitz). [161],[162] However, to date, none of these monotherapies has provided the “single bullet” that may yield optimal neuroprotection and neurological outcome. Recently combined therapies that would include the use of rt-PA together with a NADPH oxidase (NOX) inhibitor such as apocynin to blunt ROS formation and adjuvant therapy with hypothermia or ethanol (a vasodilator) have been advocated (Fujiwara et al., Fu et al., Geng et al., Zhili et al.). [163],[164],[165],[166] While these combined therapies seem promising, much work needs to be done to demonstrate their efficacy at the clinics.